Closed Loop Medicine Administration (CLMA) is the use of digital technologies (which can include use of barcode scanners, electronic patient records (EPR), electronic prescribing and medicine administration (EPMA) systems, and electronic drug cabinets) to provide additional validation when administrating medication.
This helps to ensure patients receive the correct medication in accordance with the 5 rights of medication administration: right patient, right medication, right dose, right route, right time.
The process should either generate an alert to the staff member administering the medication if there is a mismatch, or if all checks are correct an administration record should be recorded where applicable.
How Closed Loop Medicine Administration works
The process of CLMA is shown below:
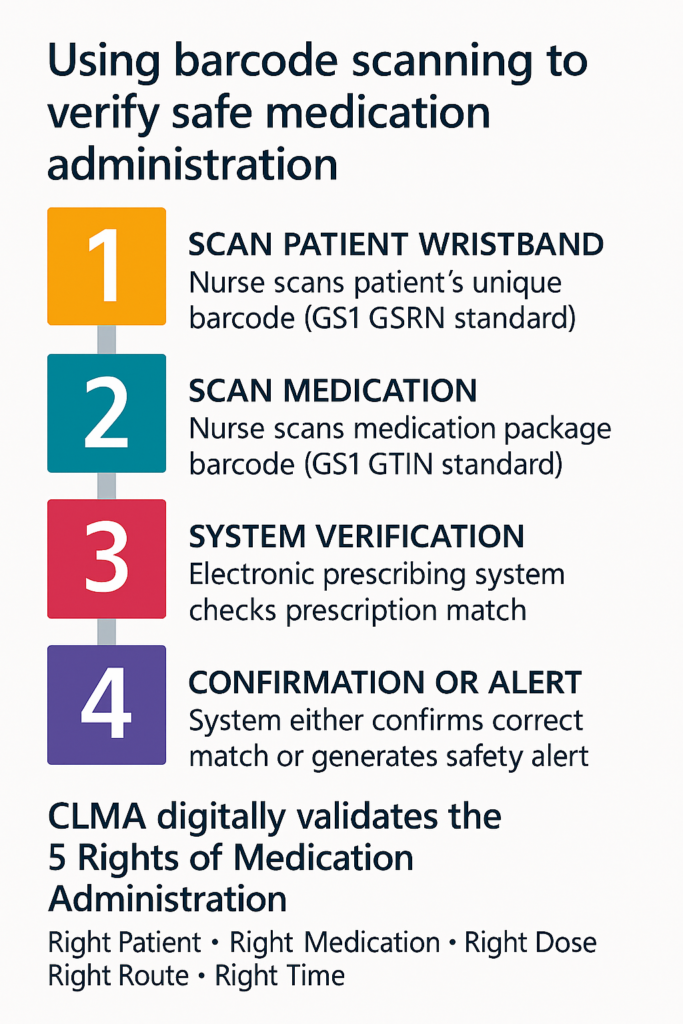
- Scan the patient: Nurse scans the patient’s wristband barcode along side the positive patient identification check (using the GS1 GSRN standard for patient identification, DCB1077: AIDC for Patient Identification, DAPB0108: Automatic Identification and Data Capture (AIDC))
- Scan the medication: Nurse scans the barcode on the medication package (using the GS1 GTIN standard for product identification)
- System verification: The electronic prescribing system confirms the match against the prescription
- Alert or confirm: The system either alerts the member of staff administering the medication if there’s a mismatch, or confirms correct administration and automatically records it in the patient record
The benefits of Closed Loop Medicines Administration
CLMA delivers significant improvements across patient safety, operational efficiency, and data quality. Evidence from NHS trusts implementing CLMA demonstrates consistent benefits that support safer medication administration and more productive healthcare delivery.
- Enhanced patient safety: CLMA technology reduces medication administration errors by digitally verifying the “five rights” of medication administration. Trusts report measurable reductions in medication errors and near-misses, with systems capturing and preventing errors that might otherwise have reached patients. This digital verification provides an additional safety layer beyond manual checks, reducing the cognitive burden on nursing staff whilst strengthening safety processes.
- Improved workflow and productivity: By automating verification processes and reducing manual documentation, CLMA releases valuable time back to clinical staff. The technology streamlines medication rounds, eliminates duplicate record-keeping, and provides real-time updates to electronic prescribing systems. This means nurses can spend more time on direct patient care rather than administrative tasks.
- Better data and analytics: CLMA systems create comprehensive data repositories that support quality improvement, compliance monitoring, and strategic decision-making. Trusts can track scanning compliance, identify trends in near-misses, and target support where needed. This data capability enables rapid identification of affected patients during medication recalls and supports ongoing service improvement through evidence-based insights.
You can also view our CLMA case studies to read real examples of how CLMA is being used by NHS trusts.
How this applies Scan4Safety principles
CLMA is a direct application of Scan4Safety principles to medicines administration. It relies on:
- GS1 standards: Using globally recognised GTIN barcodes on medications and GSRN for patient identification
- Scanning technology: Handheld scanners or mobile devices integrated with electronic prescribing systems
- Digital integration: Connecting electronic patient records, prescribing systems, and pharmacy systems
- Standards compliance: Meeting NHS standards DCB1077 (patient identification) and DAPB0108 (product identification)
CLMA Implementation considerations
Below are some specific considerations for implementing a CLMA system.
You can also read some examples of implementation approaches used by NHS trusts in our CLMA case studies.
Implementing CLMM requires understanding of how digital systems, clinical processes, and staff workflows integrate across the entire patient medication journey. We’ve developed detailed service blueprints that visualise CLMM processes at two different levels of automation – from intermediate implementation through to advanced systems incorporating automated drug cabinets.
Getting started with Closed Loop Medicines Administration
Implementing CLMA in your trust involves several key steps:
- Assess current digital maturity: Review your electronic prescribing system capabilities and integration options to assess the approach for adoption.
- Engage clinical teams: Work with nursing staff and pharmacists to understand current workflows
- Plan infrastructure: Ensure Wi-Fi coverage, device availability, and system integration
- Choose the approach for adoption: Big bang vs gradual roll out
- Pilot and learn: Start with a single ward or specialty to demonstrate benefits and refine processes
- Scale systematically: Roll out across the trust with strong change management support
Barcode challenges
Not all medications have scannable barcodes. Trusts report challenges with:
- Medications (in particular IV medication vials) where outer packaging contains the barcode rather than the individual vial.
- Barcodes damaged during transit or storage
- Specialised or unlicensed medications (particularly in paediatrics) without manufacturer barcodes
Solutions: Trusts implement pharmacy barcode labelling systems, maintain lists of exceptions, and work with suppliers to improve barcode availability.
Drug catalogue maintenance
CLMA requires an up-to-date drug catalogue mapping medication barcodes to the dm+d (dictionary of medicines and devices) standard.
Challenges include:
- New medications requiring catalogue updates
- Time required to maintain accurate drug catalogue mappings
Solutions: Dedicated pharmacy staff for catalogue maintenance, automated updates where possible, and robust business cases that include ongoing maintenance resources.
Clinical workflow integration
Successful CLMA requires thoughtful integration into clinical workflows:
- Placement of workstations or trolleys for easy access
- Wi-Fi coverage in all medication administration areas
- Scanner availability and charging infrastructure
- Clear protocols for system downtimes or failures
- Staff training and ongoing support
Closed Loop Medicines Administration and Scan4Safety
Trusts with established Scan4Safety implementation are well-positioned to adopt CLMA. The core infrastructure – GS1 and NHS standards, scanning devices, barcode-enabled patient wristbands, and digital integration provides the foundation for medicines administration scanning.
CLMA represents a natural extension of Scan4Safety principles into medication administration, one of the highest-risk clinical processes.
Closed Loop Medicines Administration case studies
The case studies below provide some real world examples of how NHS trusts have been implementing and using CLMA.
Non-urgent advice: Cambridge University Hospital NHS Trust Foundation Trust | approximately 1000 beds | Acute Secondary NHS Trust
Cambridge University Hospitals implemented Barcode Medication Administration (BCMA) to improve patient safety, with manual medication checks previously in place.
The trust’s process involves scanning both the patient’s wristband and the medication barcode and having the electronic patient record (EPR) confirm (or not) the match. BCMA supports nurses in confirming the five rights of medication administration in real time.
Processes were mapped out with nursing staff and pharmacists to create the medication administration workflow. Digitally enabled medicines management and optimisation, supported by dm+d and GS1 barcodes, enabled the introduction of a closed-loop medication management system.
This has helped alleviate adverse drug events and improve overall health outcomes for patients. The trust used data from the system to understand scanning compliance of CLMA by medication, nurse, or ward, which helped drive adoption of the new technology.
Non-urgent advice: South Tyneside and Sunderland NHS Foundation Trust | approximately 970 beds | Acute Secondary NHS Trust
Sunderland NHS Foundation Trust had already implemented an electronic prescribing system in 2009, which made CLMA implementation more challenging compared to South Tyneside. Both sites used the same approach for CLMA rollout: one ward at a time.
The process used involves scanning both the patient’s wristband and the medication barcode, with the electronic patient record (EPR) confirming the match. If patients bring in their own medication (patient own drugs – PODs), these are added to the drug catalogue on the pharmacy system to ensure recognition during scanning.
As part of their CLMA workflow, nurses are required to record a reason when they are unable to scan the medication. If the medication is not recognised on the electronic system and requires addition to the drug catalogue, the medication is returned to the pharmacy department by the pharmacy technician to ensure the system can be updated.
This approach ensures the drug catalogue remains current and issues are addressed systematically.
Non-urgent advice: Great Ormond Street Hospital | 30 wards | Paediatric NHS Trust
Great Ormond Street Hospital implemented CLMA when the trust went live with their EPIC Electronic Prescribing Record system in 2019.
As a children’s hospital, medications used by paediatric patients do not always include barcodes (e.g., unlicensed medication). The EPIC system captures data on near misses – medication errors that were prevented by the system – as well as scanning compliance. This data is used to analyse trends and identify areas that may need additional support with the system.
The rollout approach was “big bang” – the system was implemented across all wards simultaneously. Staff engagement was critical for successful rollout, involving newsletters, presenting data on how many errors were prevented, and staff feedback from surveys. Training was developed in-house for staff.
The benefits have been reduction in errors for medicine administration.
Non-urgent advice: University College London Hospitals NHS Foundation Trust (UCLH) | 665 beds | Acute Secondary NHS Trust
UCLH implemented CLMA in 2019 as part of a “big bang” rollout of the EPIC electronic health record. Patient safety was the key driver for implementing CLMA.
The process involves scanning both the patient’s wristband and the medication barcode, with the electronic patient record confirming (or not) the match.
Two workflows are available for nursing staff when using CLMA. The first workflow involves scanning the patient’s wristband, which brings up the electronic record allowing the nurse to identify what medications are required at that point in time. The second workflow involves scanning medications away from the patient bedside (e.g., in the drug treatment room if preparation is required) then scanning the patient at the bedside to complete the five rights process.
The aim of both workflows is to ensure the scanning safety component is carried out at the safest point in time. The trust does not use automated cabinets on wards; medications are stored in the drug treatment room or in patient bedside lockers.
Non-urgent advice: Alder Hey Children’s Hospital | 270 beds | Acute Secondary NHS Trust
Alder Hey Children’s Hospital implemented CLMA on all inpatient wards.
Scanning of patient wristbands is mandated; however, scanning of the medicine barcode is not. As a children’s hospital, many medications do not have barcodes as they are unlicensed. On inpatient wards, children wear patient wristbands except on the long-stay ward where photo ID is used to identify patients, with the barcode placed on the photo ID for nursing staff to use.
Medications are stored in the drug treatment room and prepared away from the patients as children sometimes get anxious when seeing needles etc. The wards have Omnicell automated cabinets for medication storage.
In house training has been developed to train staff on the process of CLMA. The trust uses dashboards created from data captured in the system to review the number of errors prevented using CLMA, as well as scanning compliance as part of the governance process within the trust.
Non-urgent advice: Oxford University Foundation Trust (OUFT) | approximately 990 beds | Acute Secondary NHS Trust
The electronic prescribing system in place at OUFT is Cerner. The process for CLMA is the patient wrist band is scanned; the medication is scanned and administer to the patient if all match against the electronic prescription.
The trust is using a one ward at a time process for the adoption of CLMA, with a new ward being implemented every 2 weeks. A dedicated roll out team was deployed to each area at go live to provide ‘elbow training’ to staff and floor walkers were available to staff during implementation.
Implementation issues the trust highlighted include patient’s own medications not having barcodes, and the inability to scan intravenous medications using the CLMA system. If a new product was procured by the pharmacy a new record would need to be produced and added onto the pharmacy drug catalogue.
Automated drug cabinets are not in place, however, this would be a future opportunity. If automated cabinets were implemented on the ward this would link to the electronic prescription that would automatically select the cabinet which had the required drug at a ward level.
Benefits have included reductions in the cognitive burden for staff and a reduction in medication administration errors.
Non-urgent advice: Newcastle upon Tyne Hospitals NHS Foundation Trust | approximately 1729 beds | Acute Secondary NHS Trust
Newcastle upon Tyne Hospitals NHS Foundation Trust has implemented CLMA using a e Cerner electronic prescribing system; however, uptake has been low.
The main reason for the low uptake is barcodes not being recognised by the system. Another challenge is that the process for uploading new barcodes to the system is not automatic. Barcodes have been built into the system manually using data captured from the dispensing robot. The drug catalogue at the trust requires an update, which is planned.
Non-urgent advice: Royal Free London NHS Foundation Trust | approximately 900 beds | Acute Secondary NHS Trust
Royal Free London NHS Foundation Trust began rolling out CLMA across their three sites in November 2018.
The processes for CLMA include use for solid oral medications, intravenous medications, and controlled drugs. The trust developed a video to demonstrate their gold standard medication administration process, providing clear guidance for staff and supporting consistent adoption across sites which is available to access here: Gold Standard Medication Administration (youtube.com)
Non-urgent advice: St George’s University Hospital NHS Foundation Trust | approximately 1300 beds | Acute Secondary NHS Trust
St George’s University Hospital NHS Foundation Trust has CLMA in place across the majority of clinical areas, including intensive care units and paediatrics wards.
Medications are stored in treatment rooms, patient bedside lockers, and workstations on wheels (WOW). The CLMA process involves nurses using barcodes on patient wristbands and medications. Controlled drugs and intravenous medicines have been excluded from the CLMA process. The drug catalogue is updated in-house.